Abstract
Objective:
To study the occurrence of portal vein thrombosis (PVT) in Omani patients.
Methods:
This is a Retrospective analysis performed on patients diagnosed with PVT which was confirmed by radiological imaging from two tertiary hospitals over a 10 year period.
Results:
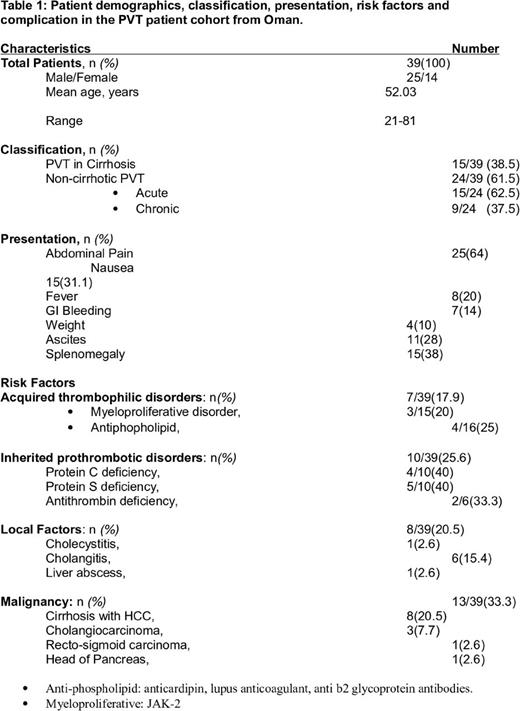
A total of 39 PVT patients were enrolled in this study, with 15(38.5%) showing cirrhosis of liver whereas, 24(61.5%) were classified as non-cirrhotic. Non cirrhotic PVT patients were further subdivided as acute or chronic; 15 (62.5%) had an acute non-cirrhotic PVT whereas the remaining 9 (37.5%) had chronic PVT. PVT were more common in males i.e. 25(64.1%) in contrast to 14(35.9%) females (p=0.02, Chi Square test). Abdominal pain in 64%, nausea in 31.1%, and fever in 20%, gastrointestinal bleeding (hematemesis or melena) 14%, and weight loss in 10%. Demonstrable ascites and splenomegaly were seen in 28% and 38% respectively. Amongst the 18 patients who were tested (majority of non-cirrhotic PVT patients) for an underlying thrombophilia, 4/10(40%) had protein C deficiency, 5/10(50%) had protein S deficiency, and 2/6(33.3%) had antithrombin deficiency. Antiphopholipid antibodies (anti-cardiolipin, lupus anticoagulant and anti-beta2 glycoprotein antibodies) were found in 4/16 (25%) patients, V617F JAK mutation was positive in 3/15 (20%) of patients. Factor V Leiden mutation, prothrombin G20210A mutation, hyperhomocystinemia, and paroxysmal nocturnal hemoglobinuria PNH (tested 7, 4, 2 and 1 patients, respectively) were all negative. Local factors were seen 8 (20.5%) patients of PVT; six had cholangitis and one patient had cholecystitis with and liver abscess. Cirrhosis of liver was the only risk factor in 15(38.5%) patients. However, 8 (53%) cirrhosis patients had hepatocellular carcinoma which is considered as risk for PVT. 13 (33.3%) patients in this study had an underlying malignancy. 8 cases were HCC all noted in cirrhosis patients. Three patients had Cholangiocarcinoma, and one patient had recto-sigmoid carcinoma, and one patient had carcinoma of head pancreas. 18(46.2%) PVT patients received immediate anticoagulation with heparin followed by warfarin, 16 patients (66.7%) were non-cirrhotic PVT. Thrombectomy was done for one patient. 7 (17.9%) patients with acute non-cirrhotic PVT had full recovery and 6(15.4%) of total PVT patients died. 26 (66.7%) patients had no detail follow up as they were lost or their care had been transferred to local hospital but we concluded their condition was stable
Conclusions:
This is the first study reflects the real life practice of portal vein thrombosis which occur due to inherited and acquired prothrombotic conditions and happen as a complications of local and malignant causes. We have studied the prevalence, clinical presentation, treatment given and outcomes. Causative factors were found in 36 patients (92.3%) of the present cohort, etiological screening seems worthwhile in every case with PVT. Significant number of PVT found to have underlying malignancies. Thrombophilia screening may not be cost-effective.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal